DermatoConnect
Cutaneous Manifestations of SARS‑CoV‑2 Infection
The number of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cases has been increasing worldwide and numerous dermatologic manifestations associated with SARS-CoV-2 infection have been reported. Estimated rates of coronavirus disease 2019 (COVID-19) related cutaneous manifestations range from 4% to 20.4%.1
Objectives
The study's objective was to review various skin manifestations brought on by SARS-CoV-2 infection.1
Methods
- The researchers used specific key words to conduct searches on PubMed.1
- In the narrative review, articles that were published between September 2014 and August 2021 were included.1
Results
| Cutaneous manifestation1 | Clinical presentations1 | Histopathology1 | Prognosis/Treatment1 |
|---|---|---|---|
| Chilblain-like or pernio-like lesions | Dusky, erythematous to oedematous papules, nodules, plaques, or, less frequently, bullae formation on acral surfaces | Superficial and deep perivascular lymphocytic infiltrate of predominantly CD3+/CD4+ T cells. Negative immunofluorescence. | Chilblain-like or pernio-like lesions are self-limiting, lasting from 10–14 days and, occasionally, for a few months. It will benefit from staying out of the cold and donning warm, protective clothing, gloves, and socks. CBLL can also benefit from pharmacological treatments, such as topical corticosteroids, topical and oral vasodilators like nitric oxide paste, oral calcium channel blockers, pentoxifylline, sildenafil, or aspirin. |
| Maculopapular or morbilliform lesions | Erythematous macules with areas of normal-appearing skin on the trunk and extremities with pruritus | Spongiotic dermatitis with eosinophils in earlier lesions, or mixed perivascular lymphocytic infiltrate with histiocytes in later lesions | Topical corticosteroids may be used to treat mild cases of pruritus. Systemic corticosteroids may be used in severe cases. |
| Urticarial lesions | Migratory, pruritic, oedematous, variably-sized wheals within 24 hours, without bruising or hyperpigmentation and/or angioedema | Perivascular lymphocytic infiltrate, scattered eosinophils, and upper dermal oedema with no virally induced cytopathic changes | These lesions might be present prior to the onset of a fever or alongside pyrexia and cough. Lesions are typically a sign of a serious illness. Second-generation antihistamines are used to treat the symptoms of SARS-CoV-2-related urticaria. Short-term use of antihistamines and steroids can improve urticaria lesions. |
| Vesicular or varicella-like lesions | Small, scattered monomorphic vesicles on the trunk with mild or absent pruritus, pain, or a burning sensation | Vacuolar degeneration of basal layer, apoptotic keratinocytes, mild inflammatory infiltrate, and multinucleated keratinocytes | Varicella-like lesions in SARS-CoV-2–infected patients have a mixed prognosis. These lesions typically receive supportive treatment. They self-resolve without leaving any scars after a few days. |
| Livedoid lesions | Livedo reticularis: symmetric, lace-like dusky patches forming pale-centred rings along blood vessels. Livedo racemosa: irregular and asymmetrical dusky patches along blood vessels | Epidermal necrosis, superficial and deep dermis thrombosis vasculopathy in small and medium vessels, sweat gland necrosis, mild perivascular lymphocytic infiltrate, and complement deposition in the vessel walls | Adults with livedoid lesions commonly require support from intensive care units. In extreme circumstances, necrosis as well as skin scabbing and sloughing may be present. For milder lesions, active non-intervention is a possibility, whereas severe cases may require everything from intensive supportive care to symptomatic treatment. |
CBLL: Chilblain-like lesions; CD3: Cluster of differentiation 3; CD4: Clusters of differentiation 4; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2; T cells: T lymphocyte.
Adapted from Huynh T, et al. Am J Clin Dermatol. 2022.
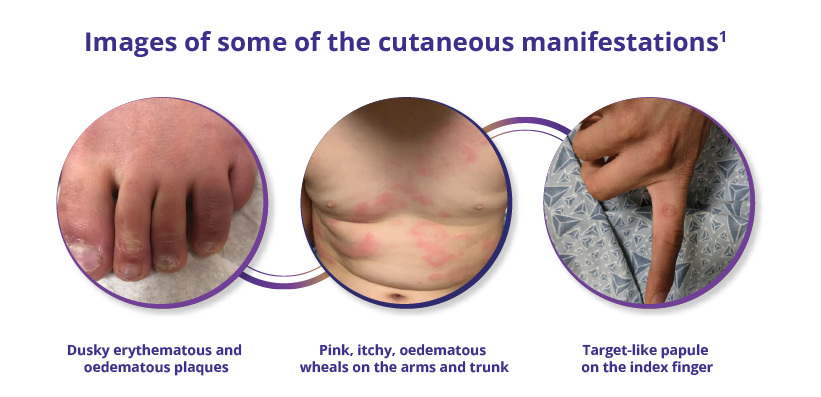
Images captured from Huynh T, et al. Am J Clin Dermatol. 2022.
Conclusions
CBLL: Chilblain-like lesions; COVID-19: Coronavirus disease 2019; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.
Referentie :
1. Huynh T, Sanchez-Flores X, Yau J, et al. Cutaneous manifestations of SARS-CoV-2
infection. Am J Clin Dermatol. 2022;23(3):277–286. https://doi.org/10.1007/s40257-022-00675-2.
NON-2023-0557 Date of creation January 2023














